N.D.V.H FOR BENIGN GYNAECOLOGICAL DISEASE - A PROSPECTIVE STUDY
ABSTRACT: OBJECTIVE
To assess safety and feasibility of non-descent vaginal hysterectomy for benign gynecological disease.
METHODS
A prospective study was conducted at the department of obstetrics and gynecology of Vydehi Medical College and research centre from January 2012 to December 2013. An effort was made to perform hysterectomies vaginally in women with benign or premalignant conditions in the absence of prolapse. A suspected adnexal pathology, Endometriosis, immobility of uterus, uterus size more than 16 weeks was excluded from the study. Vaginal hysterectomy was done in usual manner. In bigger size Uterus morcellation techniques like bisection, debulking, decoring, myomectomy, or combination of these were used to remove the uterus. Data regarding age, parity, uterine size, estimated blood loss, length of operation, intra-operative and post-operative complications and hospital stay were recorded.
RESULTS
A total of 100 cases were selected for non-descent vaginal hysterectomy. Among them 97 cases successfully underwent non-descent vaginal hysterectomy. Majority of the patients (55%) were in age group of 40-45 yrs. Four patients were nulligravida and eight patients had previous LSCS. Uterus size was ≤12 weeks in 84cases and >12-16 weeks in 16 cases. Commonest indication was leiomyoma of uterus (43%). Mean duration of surgery was 70±20.5 min. Mean blood loss was 150±65 ml. Reasons for failure to perform NDVH was difficulty in opening pouch of Douglas in two cases because of adhesions and in one cases there was difficulty in reaching the fundal myoma which prevented the uterine descent. Intra-operatively one case had bladder injury (1%) that had previous 2 LSCS. Post operatively complications were minimal which included post-operative fever (11%), UTI (8%) and vaginal cuff infection was (4%). Mean hospital stay was 3.5 days.
CONCLUSION:
Vaginal hysterectomy is safe, feasible in most of the women requiring hysterectomy for benign conditions with less complications and shorter hospital stay.

BACKGROUND:
Hysterectomy is one of the most commonly performed major operations. Hysterectomies are performed vaginally, abdominally, or with laparoscopic or robotic assistance. When choosing the route and method of hysterectomy, the physician should take into consideration how the procedure may be performed most safely and cost-effectively to fulfil the medical needs of the patient.1 Abdominal hysterectomy is undoubtedly the most popular with a 70:30 ratio for abdominal versus vaginal route.1,2 Gynecologic surgeons worldwide continue to use the abdominal approach for a large majority of hysterectomies that could be performed vaginally despite well-documented evidence that vaginal hysterectomy has distinct health and economic benefits in terms of fewer complications, better post-operative quality-of-life outcomes, and reduced hospital charges.2, 3, 4 The latest VALUE STUDY concluded that major hemorrhage, hematoma, ureteric injury, bladder injury, and anesthetic complications were more in laparoscopic assisted hysterectomy (LAVH) group when compared to abdominal and vaginal hysterectomies. In addition LAVH was accomplished in twice the time required for vaginal hysterectomy.5,6 The objective of this study was to assess the possibility of the vaginal route as the primary route for all hysterectomies for benign conditions, in the absence of uterine prolapse.
METHOD:
The study was conducted in dept. of OBG Vydehi medical college and research centre Bangalore during January 2012 to December 2013. A total of 100 patients admitted to gynecological ward requiring hysterectomy for benign diseases in the absence of uterine prolapse without suspected adnexal pathology were taken for study. Prerequisites for non descent vaginal hysterectomy (NDVH) were set as uterine size not exceeding 16 weeks of gravid uterus (by clinical judgment) and adequate vaginal access with good uterine mobility. Exclusion criteria included uterus with restricted mobility, suspicion of malignancy, complex adnexal masses. A written informed consent was taken from all patients after explaining the procedure and Special consent for conversion to abdominal hysterectomy if needed, was taken. Pre-operative investigations including complete hemogram, urine analysis, blood grouping with Rh-typing, blood sugar, serum creatinine, blood urea, Pap smear, endometrial biopsy, ECG, Chest X-ray/ USG Abdomen and Pelvis was done.
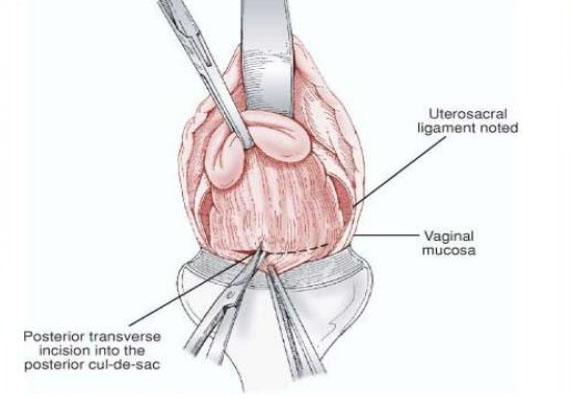
All cases were done under regional anesthesia, either spinal or epidural. All cases were re-assessed in operating theatre after patient was anaesthetized, to see the size, mobility of the uterus, vaginal accessibility and laxity of the pelvic muscles. After cleaning and draping, cervix was held with volsellum. Circumferential incision was made around the cervix, pubo-vesico-cervical ligament was cut and bladder mobilized upwards. Both anterior and posterior pouches were opened one after another. Uterosacral and cardinal ligaments were clamped, cut and ligated. Clamping of uterine vessels was done bilaterally. If at this time the uterine size did not allow an easy exteriorization then debulking techniques like morcellation, bisection, decoring, myomectomy, or a combination of these methods were done. After delivering the uterus in the vagina, hysterectomy was completed in the usual manner. VH was considered successful if it was not converted to the abdominal route.
Operating time was calculated from the start of incision at cervico-vaginal junction to the placement of vaginal pack. Blood loss was calculated by noting the number of Mops used during surgery and blood collected in suction bottle. Post-operative catheterization with Foley’s catheter was done in all cases for 24 hours. All the women received prophylactic antibiotic as per hospital protocol. Post operatively hemoglobin estimation was done and all patients were meticulously followed. Post-operative complications like fever, urinary tract infection, vaginal cuff cellulitis, vaginal bleeding is noted. All patients were followed from time of admission to time of discharge and 2 weeks thereafter. Data regarding age, parity, uterine size, estimated blood loss, length of operation, complications and hospital stay were recorded and statistically analysed using SPSS software.
RESULTS:
Among 100 patients included in the study 97 patients successfully underwent non-descent vaginal hysterectomy, whereas three cases had to be completed by abdominal route due to various reasons. Majority of the patients belonged to age group 40- 45 years. Mean age in vaginal hysterectomy group is 44.5 yrs. Age wise distribution of patients is given in table no 1.
Majority of patients were para 2 and above. Parity wise distribution of patients is given in table 2. Four patients were nulligravid. Eight patients were with previous one or two LSCS.
The commonest indication for hysterectomy was fibroid uterus 43/100 (43%). Other indications were DUB, adenomyosis, pelvic inflammatory disease, premalignant conditions of cervix, post menopausal bleeding, endometrial and cervical polyp. Patient distribution according to indication for surgery is given in table 3.
Majority of the patients had uterine size less than 12weeks 84/100 (84%). Sixteen patients had uterine size between 12-16 weeks. Uterine size wise distribution of patients is given in table 4. Different morcellation techniques like bisection, decoring, myomectomy and debulking techniques were used during the surgery to remove bigger sized Uterus Volume reduction techniques were mostly required for uterine size 12 weeks and above. Debulking techniques were done in 40/100 (40%) patients.
In the present study the mean operating time was 70±20.5 minutes. Mean blood loss was 150±65 ml. Blood transfusion was needed in 10 patients. There was bladder injury in one patient intra-operatively who had previous 2 LSCS. Mean hospital stay was 3.5 (3-7) days. Post-operative fever was seen in 11 patients, UTI in 8 patients, vaginal cuff infection was seen in 4 patients as mentioned in table 5.
DISCUSSION:
In the absence of uterine prolapse, most gynecologists prefer the abdominal to the vaginal route of hysterectomy. The common limitations for vaginal hysterectomy in non prolapsed uterus include size of the uterus, nulliparity, previous pelvic surgery or lower segment caesarean section (LSCS), pelvic adhesions and endometriosis.7The factors that may influence the route of hysterectomy for any surgical indication include uterine size, mobility, accessibility, and pathology confined to the uterus (no adnexal pathology or known or suspected adhesions).8
In the present study out of 100 cases selected for NDVH, 97cases were completed successfully, whereas three cases were converted to abdominal hysterectomy. Reasons for failure to perform NDVH was difficulty in opening pouch of Douglas in two cases because of adhesions and in one cases there was difficulty in reaching the fundal myoma which prevented the uterine descent. Majority of the patients were in the age group of 41-45 year. Similar age prevalence was noted in other case series reviews.9- 12 Similarly most of the patients were parous comparable to other studies.9-11 Lax tissues following multiple deliveries and decreased tissue tensile strength provide comfort to vaginal surgeon even in the presence of uterine enlargement. In the present study four patients (4%) were nulligravida.
A major factor in determining the route of hysterectomy is transvaginal accessibility of the uterus. Inadequate accessibility sustaining from a narrowed vagina at the vaginal apex makes vaginal hysterectomy technically challenging and may contraindicate vaginal hysterectomy, especially by surgeons less experienced in this procedure. Two factors limit accessibility an undescended, immobile uterus and a vagina narrower than 2 fingerbreadths, especially at the apex. If the vagina will allow access to divide the uterosacral and cardinal ligaments, uterine mobility usually is improved enough to allow vaginal hysterectomy in these cases.13
Determining whether the pathology is confined to or extends beyond the confines of the uterus is critical to selecting the most appropriate route of hysterectomy. The presence of severe endometriosis, adnexal pathology, adhesions because of previous pelvic surgeries contraindicate vaginal hysterectomy.14 The commonest indication was fibroid uterus (43%). Fibroid uterus was the commonest indication in other case series.9, 10, 12 In our study 16 cases had uterine size more than 12 weeks which was similar to Bandra et al11 in their study successfully removed 16/158 uterus of 12 to 20weeks size. Similar findings were reported by Unger15 who operated upon uteri weighing 200 to 700 gms without any increase in complications as compared to abdominal hysterectomies. These patients required volume reducing techniques like decoring, bisection, myomectomy or a combination of these after ligation of the uterine artery.
Mean blood loss was 150±65 ml and amount of loss depend on uterine size and duration of surgery as compared to Bhadra B et al (100ml).11 Ten patients required blood transfusion, Mean duration of surgery was 70±20.5 minutes as compared to Goel et al (64 minutes), 3 Dewan et al (54.5 minutes),4 Bharatnur et al (65minutes)10 and Bhadra B et al (55 minutes).11 The operative time was definitely more in the earlier phase of the learning curve. It was also dependent on the size of uterus and experience of the surgeon.
Our study included 8 cases with previous LSCS; Intra-operatively one case had bladder injury (1%) who had previous 2 LSCS. Bladder injury during vaginal hysterectomy has been variously reported between 0.5 to 1.6%. Unger16reported an incidence of 2.8% in the past LSCS group vs. 1.6% in those without caesarean section. Sheth17reported a very low incidence of bladder injury 7/5655 (0.1%). Post operatively complications were minimal which included post-operative pain, fever and UTI. Mean hospital stay was 3.5 days.
CONCLUSION:
The technique used for hysterectomy should be dictated by the indication for the surgery, patient characteristics, and patient preference and experience of the surgeon. Most patients requiring hysterectomy should be offered the vaginal approach when technically feasible and medically appropriate. Vaginal hysterectomy for non-descent large uterus is safe and feasible provided one is familiar with the morcellation techniques. Vaginal hysterectomy for nonprolapsed uterus should therefore be practiced more frequently by gynecologists and should be included in training programs for residents and postgraduate students.
Age Group (yrs) |
No. of Patients |
35 – 40 |
6 |
40 – 45 |
55 |
45 – 50 |
25 |
>50 |
14 |
Total |
100 |

Dr. Vikas Chhabra is Specialist in General Surgery & have 22 Yrs Experience in General, Laproscopic, Endourology, Plastic & Laser Surgeries.

Dr. Kiran Chhabra is famous Consultant of IVF, She is Specialist in Gynaecology & practicing Gynae, Obs & Infertility since 2003.

Dr. Aman Chhabra is famous Orthopedic Surgeon, He is Specialist in Ortho, Hand Surgery & Joint Replacement and have more than 15 Yrs Experience.
View More
Test Tube Baby Centre
Operation Theatre
Ventilator
ICU
OPD
Ultrasound
Colour Doppler
Laboratory
Patient Rooms
Pharmacy
24 Hours Service
Chhabra Hospital &
Test Tube Baby Centre
Near Stadium,
80 Feet Road,
Bathinda (Punjab)
Pin: 151001